Women and Children – Obstetrics and Gynaecology
Even if your surgeon has explained to you what the operation entails many of us do not take in everything mentioned in the clinic, so this information is to help you understand your condition and the reason for the intended treatment.
As we are all different, it is not possible to personalise this information, so there may be differences between your individual case and the information given here.
If you have any queries regarding the information please discuss them with the consultant or a member of their team (doctors or nursing staff).
Why do I need debulking surgery?
You are approximately half way through your plan of care and the tumour is responding to the chemotherapy so now your consultant wants to try to remove the cancer surgically. This is called debulking.
What will the operation involve?
It may be necessary to perform a laparoscopy so the surgeon can see if debulking is possible.
How is a laparoscopy performed?
A laparoscopy is a surgical procedure performed under general anaesthetic. The laparoscope is a long, pencil-slim telescope which is connected to a camera and a television system so that the inside of the abdomen can be seen magnified on a screen.
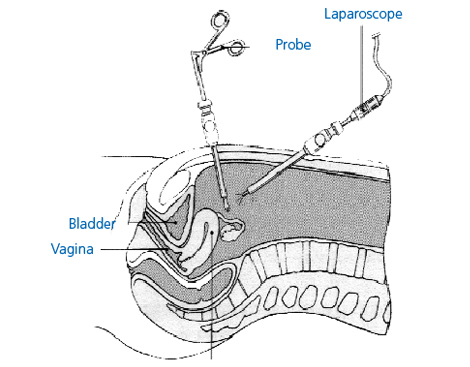
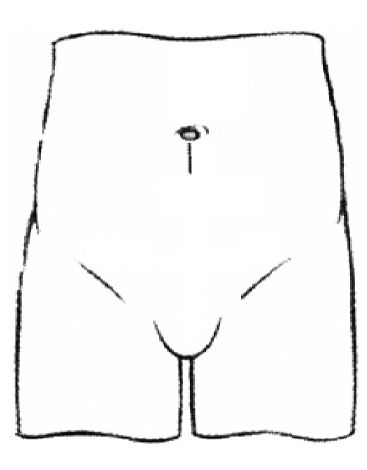
When you are asleep, a small incision (cut) is made, usually at the bottom of the umbilicus (belly button or navel). At the start of the operation, carbon dioxide gas is pumped through the incision in order to distend the abdomen. This makes sure the surgeon can clearly see the pelvic and abdominal organs during the operation.
Once the instruments are removed at the end of the laparoscopy, the gas used to inflate the abdomen is released and a stitch, or a small amount of special glue, may be put in each of the small incisions. Quite often the wound requires nothing to seal it.
If the surgeon decides there is no benefit in continuing with the debulking operation, your post-operative recovery will be the same as a diagnostic laparoscopy, and you will continue with your chemotherapy treatment.
If the surgeon decides to continue with the debulking, a laparotomy incision (cut) is then used.
How is a laparotomy performed?
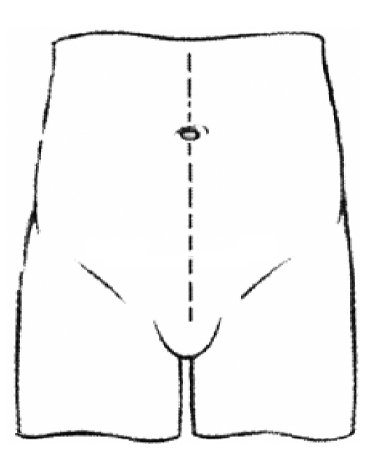
The surgeon will open the abdomen (tummy), starting at the top of the pubic hairline and going up to, and sometimes above, the umbilicus (belly button).
The exact operation depends on what the surgeon finds. Usually it will involve removal of both ovaries and tubes and removal of the womb (‘hysterectomy’). The omentum is also removed. The omentum is a pad of fat (like a baby’s bib) attached to part of the large intestine, and is a common place for ovarian cancer to spread to.
The extent of the surgery depends on how much of the cancer can be removed. In some cases it is not possible to remove much of the cancer.
Ovarian cancer can sometimes require bowel surgery, and the surgeon may make an opening inthe abdominal wall to pull through and open a section of the large bowel.
This opening is often called a stoma or colostomy. A pouch is placed over the stoma to collect the waste products that would usually pass through the bowel and out of the body through the rectum and anus (your back passage).
While this is very worrying, most patients do not need this type of surgery but it is impossible to know how extensive the surgery will be until the operation starts. The operation may also involve removal of your spleen, the spleen helps the body’s defense against bacterial infections.
The aim of the surgery is to completely remove all visible cancer (complete cytoreduction).
This is not always possible if the cancer is involved in the vital blood supply to your organs, therefore there maybe a very minimal amount of cancer left behind, (optimal cytoreduction) but this is also a good outcome from surgery.
Are there any complications or risks associated with laparoscopy or laparotomy?
We know there may be complications following various gynaecological operations or procedures, that are not particularly serious but do happen more often.
These frequently occurring risks include:
- Pain, bruising, delayed wound healing, scarring of the skin or scar tissue inside (adhesions). Numbness, tingling or burning sensation around the scar which may take weeks or months to resolve.
- Anaemia, fatigue and tiredness.
- Urinary frequency or loss of control.
- Wound infection, urinary tract infection or chest infection which is usually easily treated with antibiotics. Patients are encouraged to follow the recommended post-operative breathing exercises and to stop smoking.
Wound infection, urinary tract or vaginal infection or chest infection which is usually easily treated with antibiotics. Patients are encouraged to follow the recommended post-operative breathing exercises and to stop smoking.
Are there any ‘more serious’ risks?
It is known some risks are increased if you already have underlying medical problems or if there is scar tissue (from previous operations or disease) which makes the operation more difficult. The risks are also increased if you are obese or if you smoke.
The more serious risks include:
Pelvic abscess or infection
Occasionally an abscess may form which may require surgical drainage under an anaesthetic. All ladies having a laparotomy are given antibiotics during the operation to help prevent occurrence of infection.
Sometimes wounds do not heal as expected, this is managed individually and we are here for advice.
Bleeding
This may occur during the operation or, rarely, afterwards and may be enough to need a blood transfusion. If you have had some internal bleeding and we find blood has collected in your pelvis, we call this a haematoma.
A haematoma is often described as a blood clot, and this is quite a good description but must not be confused with the blood clots described in sections four and five. A haemotoma can usually be treated with antibiotics to encourage the blood to drain out through your vagina but occasionally it may need to be drained surgically under anaesthetic.
Visceral injury
This means injury to the bowel, bladder or ureters (the two tubes coming from the kidneys into the bladder). If there is an injury, it may need to be repaired by laparotomy. This involves a much larger abdominal incision (tummy cut) and a longer stay in hospital.
In rare cases the problem may not become apparent until a few days after the hysterectomy and this may require a second operation to resolve the problem.
Venous Thromboembolism
There are two types:
Deep vein thrombosis (DVT)
Following any gynaecological operation, it is possible for clots of blood to form in the deep veins of the legs and pelvis. If this does occur, a deep vein thrombosis would cause pain and swelling in a leg and can be treated relatively simply with drugs.
The risk of developing a DVT is minimal, as many precautions are taken to help prevent and minimise the risks such as:
- Recommending you stop your smoking in the weeks before your operation
- The use of support stockings and, or medication to ‘thin the blood‘
- The use of special equipment in the operating theatre
- Post-operative leg exercises.
Pulmonary embolism
It is possible for a clot to break away and be deposited in the lungs and if this occurs it is a serious situation and will need immediate treatment with drugs. The precautions against pulmonary embolism are the same as for DVT.
If you do have any concerns about the risk of complications, please discuss them with the consultant or a member of their team (doctors or nursing staff) and your questions will be answered as clearly and as honestly as possible.
What happens before the operation?
For this operation, you will be taking part in an enhanced recovery programme with the aim of helping you recover quickly and safely. During your short stay in hospital there will be goals which you will be encouraged to achieve.
A team of doctors, nurses, physiotherapists and other healthcare professionals will be monitoring your progress and will support you in reaching your goals.
In most cases you will be asked to attend a pre-admission session shortly before you are due to have your operation. You will be seen by a nurse who will begin your plan of care by reviewing your medical history.
You will have your weight and height, blood pressure and pulse and some blood samples taken. Depending on your age or medical history you might also be requested to attend other departments on the same day for investigations such as an ECG – Electocardiogram (heart tracing), a lung function test or a chest X-ray.
You may also need to see a doctor for a more detailed medical examination. You will need to take all your medicines to pre-admission with you as most should be continued before your operation and throughout your hospital stay but some may need to be stopped to reduce any risks and to avoid your operation being delayed or cancelled.
Your social situation and your suitability for early discharge will be discussed so this is also an opportunity for you to tell us about your own individual needs and circumstances.
It is our aim for you to have a speedy recovery and safe discharge so it is important you tell us as early as possible if you have any concerns about whether or not you will be able to manage your daily activities when you go home. You may wish to bring along a relative or close friend to pre-admission who can also be involved and support you in planning your enhanced recovery.
If it is thought you may have a high chance of needing bowel surgery during your operation, the cancer nurse specialist will arrange for you to meet certain members of the surgical team to discuss with you their involvement and plan of care. This could also involve the colorectal nurse marking your skin for a potential stoma formation. You will have the opportunity to ask the nurse any questions.
Your anaesthetist would prefer you to stop cigarette (and cannabis) smoking in the weeks before your operation, as this is known to increase the risk of anaesthetic complications, breathing difficulties, coughing, nausea and sickness and chest infection. Please avoid drinking alcohol on the evening before your operation as this may lead to dehydration.
To reduce the possibility of skin infection, we request you do not shave your bikini-line or your legs during the week before your operation but some ‘trimming back’ of excess pubic hair may be required, you can do this yourself at home or the nursing staff will help you after you are admitted.
Which medicines should I take into hospital?
It is important you use the bag supplied at pre-admission to bring all your medicines with you, in their original containers, so they can be continued without delay.
You should include all:
Medicines that have been prescribed for you
Medicines that have been bought by yourself or for you
Inhalers, ear drops, eye drops, creams etc
Herbal medicines
Eating and drinking before coming into hospital
On the day before your surgery you will be able to eat and drink as normal.
A key aspect of the enhanced recovery programme is that you will be given clear carbohydrate drinks before your surgery. These drinks will help to give you the much needed energy which you will need to help you recover. A seperate instruction leaflet will be given to you at pre assessment.
Admission into hospital
Please follow your fasting instructions
Do not suck sweets or chew gum.
As you will be admitted on the day of your operation, you will need to take a bath or shower at home and take off as much of your jewellery as possible although we are able to cover wedding rings or bangles if you are unable to remove them.
To reduce the possibility of any damage to your eyes, it is very important you remove all mascara and wear glasses instead of any type of contact lenses. Please wear comfortable clothes that are not tight around the waist.
You will need to bring a packet of sanitary towels into hospital with you, toiletries, dressing gown, nightgown and slippers, and you may also choose to bring in a book or magazine.
Please read your admission letter carefully to see where you are being admitted too. If you are unsure, you may phone the nursing staff as follows:
The Surgical Admissions Unit at The James Cook University Hospital: 01642 854603
If you have not already signed your consent form for the operation, you will be seen by your consultant or a member of their team who will explain your operation in detail and answer any questions you may have. You will then be required to sign the consent form.
Because of the extent of the surgery it may be advised that you have a spinal or epidural anaesthetic. This will depend on discussion between you and your anaesthetist. You will still be sedated but a spinal (epidural) may be advised, helping to reduce the risk of a blood clot developing in your legs during the operation.
You will then be transferred to the theatre area by a nurse and or porter.
What can I expect after the operation
When the operation is completed you will be woken by the anaesthetist and transferred, on your trolley, to the recovery area in theatre. Your recovery nurse will look after you and stay with you until they are satisfied with your condition.
You will be transferred to the ward on your trolley and the ward staff, with the help of the theatre porter, will transfer you into your bed. You will probably feel drowsy for a few hours afterwards.
Although you are likely to have a ‘drip’ (also known as an I.V.), to give you intravenous fluids, it is important that you start drinking and eating early after the operation. We will encourage you to drink and even have something light to eat a few hours after your return to the ward if you are not feeling sick and only if the doctor has advised this.
You will have been given anti-sickness medication during the operation and a small tube may be placed in your nose to keep your tummy empty following the surgery, this helps to rest your bowel.
Post-operative pain is often managed with a PCA (Patient Controlled Analgesia) device that allows you to control the amount of pain relief that you receive and should result in a comfortable postoperative recovery.
The PCA and the ‘drip’, are usually removed during the first day after your operation, when the medical team feel you are ready to progress onto painkillers given by mouth or in suppository form.
Alternatively you may have a drip in your back (epidural) which allows a continuous supply of pain relieving medication to be given. This is usually removed two days after your surgery, and you will then be offered other effective pain killers.
You may also have small tubes in your wound called pain quells which give local anaesthetic cover over a few days.
Effective pain and sickness control is an important part of the enhanced recovery programme as this will allow you to start walking around, breathe deeply, eat and drink, feel relaxed and sleep well.
You may have had a catheter inserted into the bladder. This is a very slim rubber tube which drains urine from the bladder so that:
a) you do not have to get up to go to the toilet when you may still be feeling a bit drowsy and sore
b) we can make sure that the kidneys are working well.
The catheter is usually removed once mobile, usually 24 to 48 hours post op. You may have a drainage tube, leading from your abdomen, to help drain away any excess fluid. This tube is usually removed after two to three days.
To enhance your recovery it is important you start doing the recommended breathing exercises, as described in the back of this booklet, as soon as you wake up and the staff will help you out of bed. You may also be given extra oxygen to breathe after the operation until you are up and about.
You will be encouraged to increase your mobility gradually during the day after your operation until you are fully mobile making it possible for you to have a shower or to go in the bath, with some assistance from the staff.
You may feel much more tired than usual after your operation as your body is using a lot of energy to heal itself. You may need to take a nap for the first few days. A laparotomy can also be emotionally stressful and many women feel tearful and emotional at first – when you are tired these feelings can seem worse. For many women this is often the last symptom to improve.
It usually takes a few days before your bowels start to work normally and you may experience discomfort associated with a build-up of wind. This usually resolves itself, but if it becomes a problem the nursing staff may provide some peppermint water to drink and encourage taking gentle exercise.
It is important to keep your genital area and any abdominal wounds clean. A daily bath or shower is advisable paying particular attention to these areas. Avoid the use of highly scented soaps, bubble bath and vaginal deodorants, etc.
The nursing staff will provide a separate sterile towel to dry the wound and a sterile dressing to cover the wound after bathing. If dressings are still needed on discharge they will provide them.
You may have dissolving sutures (stitches) in your wound, in which case you will be advised by the nursing staff how to care for them. If you have clips, staples or sutures which need to be removed, the nursing staff will explain how to care for your wound and advise you when they will be removed.
You may have some vaginal bleeding in the first few days after the operation. The bleeding normally turns into a red or brownish discharge before stopping completely and can last anything from a few days to a few weeks.
If bleeding becomes heavier than a period or smells very offensive, let the doctor or nursing staff know as it may mean that you have an infection.
We advise you to use sanitary towels in preference to tampons whilst the bleeding persists, as this will help you to keep a check on the amount you are losing and will help to reduce the risk of infection associated with tampon use.
Some further, slight, bleeding may occur about four to six weeks after your operation. This can happen because your internal stitches are dissolving. As long as this bleeding only lasts for a day or two do not worry, but if it becomes very heavy and you are worried, please contact your GP.
How long can I expect to be in hospital after the operation?
Many patients feel well enough to leave hospital after a few days but this could lead up to 2 weeks or more dependiing on the extent of surgery. You must tell your nurse how you are feeling and she will help you to decide whether you are ready.
How will my care continue?
After your operation, the tissues taken away will be fully analysed then discussed at our Multidisciplinary Team (MDM) meeting and this usually takes up to four weeks.
We will have asked you, at pre assessment, how you would like to receive your results, either by a formal visit to out-patients clinic or by a telephone call from the specialist nurse.
A further appointment will be made for you to continue with your chemotherapy as planned. If you have any questions, please ask any of the team looking after you – we are happy to help.
If you need to contact us
If you need to contact us, please feel free to do so. The Cancer Nurse Specialist is happy to speak to you at any time. Her number is 01642 282418. If she is not there, an answerphone is available.
What happens when I go home?
You will take home the medicines you brought in with you. We will provide any extra medicines you may need, such as painkillers or antibiotics, from the hospital pharmacy. Please stock up on paracetamol and ibuprofen, if you are able to take them as we do not provide them on discharge.
We usually provide some laxatives as constipation can be a problem post op and also 28 days of heparin injections to thin the blood to help prevent deep vein thrombosis or pulmonary embolus. The nurses will discuss administration of the injections on discharge.
You will go home wearing your ‘support socks’ and are advised to wear them for two weeks when you can remove them to shower and wash and then for the next four weeks in bed at night, until you are back to your full mobility.
Many women lose their interest in sex during cancer treatment and any type of gynaecological operation can also affect our sex lives. You should usually allow six weeks after your operation to allow your scar to heal. It is then safe to have sex – as long as you feel comfortable. If you experience any discomfort or dryness you may wish to try a vaginal lubricant. You can buy this from your local pharmacy.
What can help me recover?
Rest
Rest as much as you can for the first few days after you get home. It is good to relax, but avoid crossing your legs for too long when you are lying down.
Rest doesn’t mean doing nothing at all throughout the day, as it is important to start exercising and doing light activities around the house within the first few days.
A pelvic-floor muscle exercise programme
Your pelvic-floor muscles span the base of your pelvis. They work to keep your pelvic organs in the correct position (prevent prolapse), tightly close your bladder and bowel (stop urinary or anal incontinence) and improve sexual satisfaction.
It is important for you to get these muscles working properly after your operation, even if you have stitches. To identify your pelvic-floor muscles, imagine you are trying to stop yourself from passing wind or you could think of yourself squeezing tightly inside your vagina. When you do this you should feel your muscles ‘lift and squeeze’.
It is important to breathe normally while you are doing pelvic-floor muscle exercises. You may also feel some gentle tightening in your lower abdominal muscles. This is normal. Women used to be told to practise their pelvic-floor muscle exercises by stopping the flow of urine midstream. This is no longer recommended, as your bladder function could be affected in the longer term.
You need to practise short squeezes as well as long squeezes:
- Short squeezes are when you tighten your pelvic-floor muscles for one second and then relax.
- Long squeezes are when you tighten your pelvic-floor muscles, hold for several seconds and then relax.
Start with what is comfortable and then gradually increase – aiming for ten long squeezes, up to ten seconds each, followed by ten short squeezes.
You should do pelvic-floor muscle exercises at least three times a day. At first you may find it easier to do them when you are lying down or sitting. As your muscles improve, aim to do your exercises when you are standing up.
It is very important to tighten your pelvic-floor muscles before you do anything that may put them under pressure, such as lifting, coughing or sneezing.
Make these exercises part of your daily routine for the rest of your life. Some women use triggers to remind themselves such as, brushing their teeth, washing up or commercial breaks on television.
Straining to empty your bowels (constipation) may also weaken your pelvic-floor muscles and should be avoided. If you suffer from constipation or find the pelvic-floor muscle exercises difficult, you may benefit from seeing a specialist women’s health physiotherapist.
A daily routine: Establish a daily routine and keep it up. For example, try to get up at your usual time, have a wash and get dressed, move about and so on. Sleeping in and staying in bed can make you feel depressed. Try to complete your routine and rest later if you need to.
Eat a healthy balanced diet: Ensure that your body has all the nutrients it needs by eating a healthy balanced diet. A healthy diet is a high-fibre diet (fruit, vegetables, wholegrain bread and cereal) with up to two litres a day of fluid intake, mainly water. Remember to eat at least five portions of fruit and vegetables each day. You will only gain weight if you eat more than you need to and you are not exercising enough.
Keep your bowels working: Your bowels may take time to return to normal after your operation. Your motions should be soft and easy to pass. You may initially need to take laxatives to avoid straining and constipation. You may find it more comfortable to hold your abdomen (provide support) the first one or two times your bowels move.
If you do have problems opening your bowels, it may help to place a small footstool under your feet when you are sitting on the toilet so your knees are higher than your hips. If possible, lean forwards and rest your arms on top of your legs to avoid straining.
Stop smoking: Stopping smoking will benefit your health in all sorts of ways such as lessening the risk of a wound infection or chest problems after your anaesthetic. By not smoking – even if it is just while you are recovering – you will bring immediate benefits to your health.
If you are unable to stop smoking before your operation, you may need to bring nicotine replacements for use during your hospital stay. You will not be able to smoke or use vaping devices in hospital. If you would like information about a smoking cessation clinic in your area speak with the nurse in your GP surgery.
Support from your family and friends: You may be offered support from your family and friends in lots of different ways. It could be practical support with things like shopping, housework or preparing meals. Most people are only too happy to help – even if it means you having to ask them!
Having company when you are recovering gives you a chance to say how you are feeling after your operation and can help to lift your mood. If you live alone, plan in advance to have someone stay with you for the first few days when you are at home.
A positive outlook: Your attitude towards how you are recovering is an important factor in determining how your body heals and how you feel in yourself.
You may want to use your recovery time as a chance to make some longer term positive lifestyle choices such as: starting to exercise regularly if you are not doing so already and gradually building up the levels of exercise that you take.
Eating a healthy diet: if you are overweight it is best to eat healthily without trying to lose weight for the first couple of weeks after the operation. After that you may want to lose weight by combining a healthy diet with exercise.
Whatever your situation and however you are feeling, try to continue to do the things that are helpful to your long-term recovery.
What can slow down my recovery?
It can take longer to recover from a laparotomy if you had health problems before your operation; for example, women with diabetes may heal more slowly and may be more prone to infection. If you smoke; some women who smoke are at increased risk of getting a chest or wound infection during their recovery: smoking can delay the healing process.
If you were overweight at the time of your operation it can take longer to recover from the effects of anaesthesia and there can be a higher risk of complications such as infection and thrombosis. It can also take longer to recover if there were any complications during your operation.
Recovering after an operation is a very personal experience. If you are following all the advice you have been given but do not think you are at the stage you ought to be, talk with your GP.
When should I seek medical advice after a laparotomy?
While most women recover well after a laparotomy, complications can occur – as with any operation. You should seek medical advice from your GP, the hospital where you had your operation, NHS Direct or NHS 24 if you experience:
- Burning and stinging when you pass urine or pass urine frequently: this may be due to a urine infection. Treatment is with a course of antibiotics.
- Heavy or smelly vaginal bleeding or bleeding which starts again: if you are also feeling unwell and have a temperature (fever), this may be because of an infection or a small collection of blood at the top of the vagina, called a vault haematoma.
Treatment is usually with a course of antibiotics. Occasionally you may need to be admitted to hospital for the antibiotics to be administered intravenously (into a vein). Rarely, this may need to be drained. - Red and painful skin around your scars: this may be caused by a wound infection. Treatment is with a course of antibiotics.
- Increasing abdominal pain: if you also have a temperature (fever), have lost your appetite and are vomiting, this may be because of damage to your bowel or bladder, in which case you will need to be admitted to hospital.
- A painful, red, swollen, hot leg or difficulty bearing weight on your legs: this may be caused by a deep vein thrombosis (DVT). If you have shortness of breath, chest pain or cough up blood, it could be a sign that a blood clot has travelled to the lungs (pulmonary embolus). If you have these symptoms, you should seek medical help immediately.
Getting back to normal
Around the house
While it is important to take enough rest, you should start some of your normal daily activities when you get home and build up slowly. You will find you are able to do more as the days and weeks pass.
It is helpful to break jobs up into smaller parts, such as ironing a couple of items of clothing at a time and taking rests regularly. You can also try sitting down while preparing food or sorting laundry. For the first one to two weeks you should restrict lifting to light loads such as a litre bottle of water, kettles or small saucepans.
You should not lift heavy objects, such as full shopping bags or children, or do any strenuous housework like vacuuming, until three to four weeks after your operation, as this may affect how you heal internally.
Try getting down to your children rather than lifting them up to you. If you feel pain you should try doing a little less for another few days.
Remember to lift correctly by having your feet slightly apart, bending your knees, keeping your back straight and bracing (tightening or strengthening) your pelvic floor and stomach muscles as you lift. Hold the object close to you and lift by straightening your knees.
Exercise
While everyone will recover at a different rate, there is no reason why you should not start walking on the day you return home. You should be able to increase your activity levels quite rapidly over the first few weeks. There is no evidence that normal physical activity levels are in any way harmful and a regular and gradual build-up of activity will assist your recovery.
If you are unsure, start with short steady walks close to your home a couple of times a day for the first few days. When this is comfortable you can gradually increase the time while walking at a relaxed steady pace. Many women should be able to walk for 30 to 60 minutes after two or three weeks.
Swimming is an ideal exercise that can usually be resumed within two to three weeks as long as vaginal bleeding and discharge has stopped. If you build up gradually the majority of women should be back to previous activity levels within four to six weeks.
Driving
You should not drive for 24 hours after a general anaesthetic. Each insurance company will have its own conditions for when you are insured to start driving again. Check your policy.
Before you drive you should be:
Free from the sedative effects of any painkillers
Able to sit in the car comfortably and work the controls
Able to wear the seatbelt comfortable
Able to make an emergency stop
Able to comfortably look over your shoulder to manoeuvre
In general, it can take six weeks before you are able to do all of the above. It is a good idea to practise without the keys in the ignition. See if you can do the movements you would need for an emergency stop and a three-point turn without causing yourself any discomfort or pain. When you are ready to start driving again, build up gradually, starting with a short journey.
Travel plans
If you are considering travelling during your recovery, it is helpful to think about:
- The length of your journey: journeys over four hours where you are not able to move around (in a car, coach, train or plane) can increase your risk of deep vein thrombosis (DVT). This is especially so if you are travelling soon after your operation.
- How comfortable you will be during your journey, particularly if you are wearing a seatbelt.
Overseas travel:
- Would you have access to appropriate medical advice a your destination if you were to have a problem after your operation?
- Does your travel insurance policy cover any necessary medical treatment in the event of a problem after your operation?
- Are your plans in line with the levels of activity recommended in this information?
Returning to work
Everyone recovers at a different rate, so when you are ready to return to work will depend on the type of work you do, the number of hours you work and how you get to and from work.
You may experience more tiredness than normal after any operation, so your return to work should be like your return to physical activity, with a gradual increase in the hours and activities at work. If you have an occupational health department they will advise on this.
Some women are fit to work after three to four weeks and will not be harmed by this if there are no complications from surgery. Many women are able to go back to normal work after six to eight weeks if they have been building up their levels of physical activity at home.
Returning to work can help your recovery by getting you back into your normal routine again. Some women who are off work for longer periods start to feel isolated and depressed. You do not have to be symptom free before you go back to work. It is normal to have some discomfort as you are adjusting to working life.
It might be possible for you to return to work by doing shorter hours or lighter duties and building up gradually over a period of time. Consider starting partway through your normal working week so you have a planned break quite soon.
You might also wish to see your GP or your occupational health department before you go back and do certain jobs – discuss this with them before your operation. You should not feel pressurised by family, friends or your employer to return to work before you feel ready. You do not need your GP’s permission to go back to work. The decision is yours.
Recovery tracker
| Days after operation | How might I feel? | What is safe to do? | Fit to work? |
| 1 to 2 days | You will have some pain and discomfort in your abdomen. You may feel sore moving in and out of bed. You may have some bleeding like a light period. Laparoscopy only: You will go home the next morning Laparotomy: You are likely to be in hospital during this time. | Get up and move about. Go to the toilet. Get yourself dressed. Start eating and drinking as usual. You will feel tired and perhaps feel like a sleep in the afternoon. | No |
| 3 to 7 days | You should be at home by now. Your pains should be reducing in intensity now and you will be able to move about more comfortably. You will still tire easily and may require a nap during the day. | Continue as days 1 to 4. Go for short walks. Continue with exercises that have been recommended to you. Wash and shower as normal. Have a rest or sleep in the day if you need to. | No |
| 1 to 2 weeks | There will be less pain as you move about and you will find your energy levels slowly returning. Bleeding should have settled or be very little. | Build up your activity slowly and steadily. Restrict lifting to light loads. | No |
| 2 to 4 weeks | There will be even less pain now as you move about more and more. You will find your energy levels returning to normal. You should feel stronger every day. | Continue to build up the amount of activity you are doing towards your normal levels. You can start to do low impact sport. Make a plan for going back to work. | No |
| 4 to 6 weeks | Almost back to normal. You may still feel tired and need to rest more than usual. | All daily activities including lifting. Usual exercise. Driving. Have sex if you feel ready. | Yes, if you don’t feel ready to go to work, talk to your GP or employer about the reasons for this |
Breathing exercises
The recommended breathing exercises mentioned should help maintain a clear chest, tone up muscles and ease wind pain following surgery. Start this exercise as soon as you wake up from the anaesthetic and do regularly until you increase your walking.
Bend your knees up with feet flat on the bed, breathe in through your nose until your lungs are as full as possible, then relax as you breathe out through your mouth. Repeat five times every half hour or so, and follow with two huffs.
Huff: Position as above with hands or pillows supporting any area of discomfort. Take a medium breath in, then force the air out quickly through an open mouth, as though you are trying to mist up a large mirror. Follow this with a cough – take a big breath in first, and do not worry about this doing any damage in the area of your surgery.
Foot and knee exercises
These should help the circulation and help prevent clots from forming in your legs. Repeat every time you do your breathing exercises and until you are walking about. Bend feet up and down at the ankle firmly and quickly. Draw circles with your feet. Press back of the knees into the bed and tighten up the thigh muscles.
We hope you have found this information helpful.
Ova the rainbow

Ova The Rainbow is a support group for anyone who would like support for themselves or their friends and family due to any gynaecological cancer.
It was established at the end of 2001 by two specialist oncology nurses, Jane McNeil and Lynne Wright out of The James Cook University Hospital. The Friarage branch was established in 2005 by Maggie Wright.
We are a registered charity and our meetings are held monthly for friends, family and any other supporters.
First Tuesday of the month, 2pm to 3:30pm
Allerton Court Hotel, Darlington Road, Northallerton, North Yorkshire DL6 2XF
For further details please contact: 01642 282418
Contact information:
- Gynaecology outpatients department: 01642 854243
- Surgical admissions unit: 01642 854603
- Gynae oncology nurses (Monday – Friday 8.30am-5pm): 01642 282418
Acknowledgements: The Royal College of Obstetricians and Gynaecologists
The Royal College of Obstetricians and Gynaecologists guidance on recovering well can be accessed by visiting the RCOG website
The National Institute for Health and Clinical Excellence guidance on laparoscopic radical hysterectomy may be accessed by visiting the NICE website
The Jo’s cervical cancer trust website may be a helpful resource
Patient experience
South Tees Hospitals NHS Foundation Trust would like your feedback. If you wish to share your experience about your care and treatment or on behalf of a patient, please contact The Patient Experience Department who will advise you on how best to do this.
This service is based at The James Cook University Hospital but also covers the Friarage Hospital in Northallerton, our community hospitals and community health services.
To ensure we meet your communication needs please inform the Patient Experience Department of any special requirements, for example; braille or large print.
T: 01642 835964
E: [email protected]